Pharmaceutical Stewardship in LMICs: Key to Sustainable AMR Control
Antimicrobial resistance (AMR) is one of the most challenging health issues of the 21st century, with the potential to undo decades of gains in medicine. Perhaps nowhere is the problem more pronounced than in low- and middle-income countries (LMICs), where there has been uncontrolled sale and rampant use of antibiotics that has provided rich soil for resistant bacteria to spread. The mounting crisis calls for prompt, concerted actionŌĆömost urgently through the creation and strengthening of pharmaceutical stewardship programs. Pharmaceutical stewardship in LMICs is not only a strategic imperative but an integral requirement for long-term AMR control, aligned with the overall aspirations of healthcare development and public health security.
The AMR Landscape in LMICs: A Complex Challenge
Infectious diseases disproportionately affect low- and middle-income nations, which is frequently made worse by shoddy healthcare systems and lax enforcement of regulations. These elements play a part in the widespread and frequently careless use of antibiotics. The World Health Organisation (WHO) estimates that more than 70% of antibiotic use worldwide takes place in LMICs, with a large portion of this usage taking place without a prescription or proper medical supervision. Inappropriate antibiotic use is encouraged by this unrestricted access and inadequate diagnostic tools, which can range from improper dosage and duration to completely unnecessary use.
The effects transcend the level of individual treatment failure. AMR leads to increased durations of illness, higher mortality, and higher healthcare expenditure. AMR has been estimated by the World Bank to lead to a 3.8% loss in world GDP by 2050 if left unchecked, disproportionately affecting LMICs with weak economies. These economies may not have economic buffers to withstand such shocks, and therefore AMR control is important not only from a clinical perspective but also for long-term development.
The Role of Unregulated Antibiotic Sales in Driving Resistance
Among the key drivers of AMR in LMICs is the existence of over-the-counter sales of antibiotics without prescriptions. Pharmacies and non-formal drug vendors are commonly dispensing antibiotics owing to consumer pressure, profit motives, and poor regulatory environments. A research in The Lancet Infectious Diseases pointed out that in most LMIC cities, antibiotic sales are as much as 60% without the consultation of professional medical practitioners. This issue is compounded by a lack of public awareness regarding the risks of misuse and self-medication being the cultural norm.
The presence of poor-quality and counterfeit antibiotics is an added challenge to stewardship initiatives. Inadequate drugs, which are common in black markets, are the cause of failures in treatment and resistant strain selection. This is a vicious cycle with two challenges: misuse and poor drug quality, which erode the effectiveness of present antibiotics and jeopardises future possibilities.
Defining Pharmaceutical Stewardship and Its Imperatives
Pharmaceutical stewardship entails systematic measures for optimising the use of medicines, particularly antibiotics, in order to improve patient outcomes while reducing harm, including resistance. This broad strategy includes regulation, education, supply chain management, and promotion of rational prescribing. In LMICs, pharmaceutical stewardship needs to be adapted to fit specific challenges like resource shortages, varied healthcare delivery models, and differences in health literacy.
Fundamentally, stewardship is designed to make sure that antibiotics are only prescribed when needed, in adequate quantities, and for the right amount of time. Stewardship also entails the tightening of pharmaceutical regulations to end unauthorized sales and improving the ability of healthcare practitioners through on-going education. Notably, stewardship goes beyond healthcare settings to the communities, where pharmacists, street drug sellers, and even patients play a part.
Implementing Stewardship Programs: Evidence from LMICs
Several LMICs have made substantial progress towards pharmaceutical stewardship by combining surveillance, policy, and education to effectively tackle AMR. These examples demonstrate the promise and problems of applying stewardship at scale.
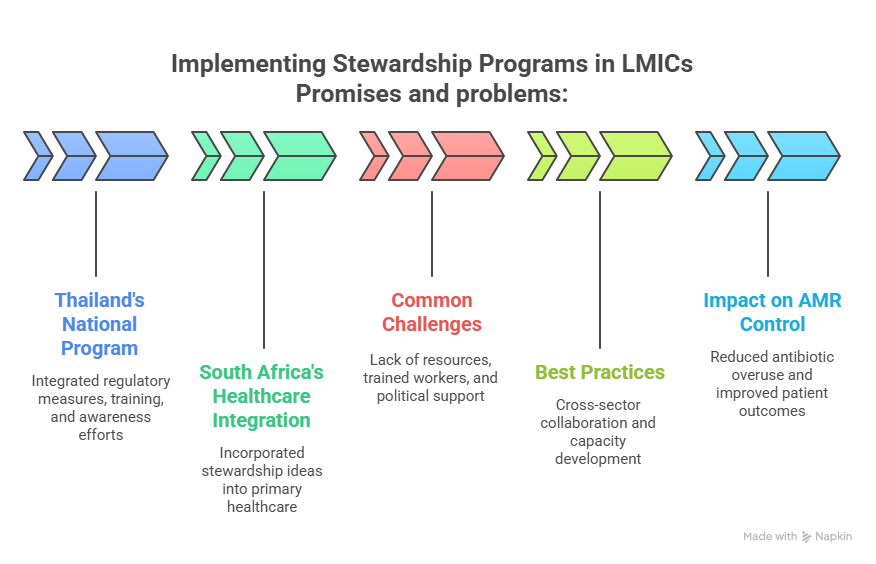
- ThailandŌĆÖs National Antimicrobial Stewardship Program: incorporated regulatory measures, healthcare professional training, and public awareness efforts.┬Ā This multimodal approach resulted in a significant reduction in antibiotic consumption and resistance rates among major pathogens, indicating the effectiveness of coordinated stewardship measures.
- South Africa’s Primary Healthcare Integration: initiative aimed to incorporate stewardship ideas into the frontline healthcare system.┬Ā Improvements included increased diagnostic capacity and stronger pharmaceutical supply chains, which all contributed to more rational antibiotic prescribing and use.
- Common challenges in LMIC stewardship efforts: include a lack of financial resources, a paucity of trained healthcare workers, and insufficient political support.┬Ā These barriers underline the importance of long-term investment and policy assistance to maintain momentum and scalability.
- Best Practices for Successful Stewardship: highlight cross-sector collaboration among government agencies, healthcare providers, chemists, and community partners.┬Ā Capacity development, ongoing education, and health information systems for real-time surveillance are key components.
- Impact on AMR Control: Stewardship initiatives have reduced antibiotic overuse, slowed the emergence of resistance patterns, and improved patient outcomes.┬Ā These accomplishments highlight the importance of stewardship in long-term AMR management.
The Economic and Public Health Rationale for Stewardship
Pharmaceutical stewardship in LMICs is a sound economic and public health investment. AMR-related infections contribute approximately billions of dollars each year to healthcare expenses with longer hospitalisation, intensive care, and the requirement for costly second- or third-line antibiotics. Inappropriate use of antibiotics is reduced through stewardship, saving the efficacy of current drugs and preventing the transmission of resistant infections.
In addition, stewardship advances public health objectives by enabling safer, more efficient healthcare practices. Not only does AMR complicate therapy but also threatens standard procedures like surgeries and chemotherapy, which depend on prophylactic antibiotics that work. In LMICs, where infectious diseases continue to be a major cause of morbidity and mortality, stewardship plays a pivotal role in protecting such gains.
Integrating Stewardship into Sustainable Healthcare Development
Pharmaceutical stewardship ought to be examined in terms of sustainable healthcare development. The United Nations’ Sustainable Development Goal (SDG) 3.3 aims directly at the elimination of infectious diseases, with SDG 3.8 aiming at universal health coverage and access to quality medicines. Stewardship programs serve directly to advance these aims by ensuring proper antibiotic use, expanding access to quality medicines, and strengthening health system resilience.
Most importantly, sustainable stewardship requires intersectoral coordination. Ministers of health, regulatory bodies, professional organisations, the pharmaceutical sector, and civil society need to work together. Investing in health information systems for tracking antibiotic consumption and resistance patterns is essential. Moreover, community mobilisation and behaviour change programs are important to change people’s attitudes and practices towards consuming antibiotics.
Challenges and the Path Forward
All too often, pharmaceutical stewardship in LMICs is hampered by significant challenges. There is weak regulation with inconsistent enforcement because of constrained resources and competing demands. Shortages of health workers and training gaps impede following the guidelines. Cultural issues such as distrust in formal health care and deeply ingrained self-medication practices undermine behaviour change interventions.
These challenges must be met with innovative, locally adapted solutions. Capacity development aimed at equipping healthcare practitioners with diagnostic resources and stewardship skills is paramount. Digital health technologies present promising pathways for surveillance and education. Global partnerships and financing arrangements must also place stewardship on the pedestal of AMR control and health system strengthening.
Conclusion
Pharmaceutical stewardship in the LMICs is categorically the pillar of sustainable AMR control. It confronts the underlying drivers of resistance by encouraging rational use of antibiotics and containing uncontrolled sales, thus maintaining the efficacy of currently available antimicrobial agents. While the LMICs face the double burden of infectious diseases and emerging resistance, stewardship programs need to be placed centrally in national health agendas and backed by strong policy frameworks, education, and community activation.
Ultimately, pharmaceutical stewardship is not so much a technical interventionŌĆöit’s a strategic bet on the future of global health. By integrating stewardship into sustainable healthcare development, LMICs can protect the effectiveness of antibiotics, enhance health outcomes, and ensure economic security against the pernicious threat of AMR. The moment for bold action is now, and stewardship programs are the cornerstone on which strong, equitable healthcare systems will be constructed.
┬Ā




















