Dental care has moved well beyond fillings and routine cleanings. In the past few years, the field has seen fast-moving advances across regenerative medicine, digital manufacturing, artificial intelligence (AI) and minimally invasive therapies. These breakthroughs promise better diagnostics, faster and more personalised treatments, and — in some cases — the possibility of restoring natural tooth structures rather than simply replacing them. Below, we’ll look at the most important recent developments, explain how they work and note what they mean for patients and clinicians.
Regenerative dentistry: repairing rather than replacing
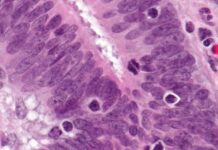
One of the most exciting areas is regenerative dentistry, which uses stem cells, tissue engineering and advanced biomaterials to encourage the body to rebuild damaged tooth and periodontal tissues. Researchers have reported promising results using dental pulp stem cells and related cell types to regenerate pulp tissue and repair periodontal defects. Early clinical studies have suggested that allogeneic dental pulp stem cell injections can promote periodontal regeneration in advanced cases of periodontitis, improving tissue health where conventional approaches struggle. These kinds of therapies aim to restore function and sensation, not just structural support — a paradigm shift from replacement toward true biological repair.
Despite the promise, regenerative approaches are still largely in clinical trials or early clinical use. Challenges include ensuring consistent cell quality, preventing immune reactions, integrating new tissue with existing anatomy, and navigating regulatory approval. That said, the pace of research means regenerative options could become more widely available over the coming decade, particularly for patients who would otherwise need complex implants or extensive periodontal surgery.
Tooth and tissue engineering: growing complex structures
Beyond cellular injections, tissue engineering studies have shown the potential to grow tooth-like structures in lab animals by activating resident stem cells or by seeding scaffolds with dental stem cells. Scientists are investigating scaffolds and growth-factor cocktails that encourage formation of dentine, pulp and — in some experimental settings — enamel-like tissues. If replicated in humans, these techniques could eventually provide alternatives to dental implants or dentures for replacing missing teeth, by encouraging a patient’s own tissues to form a new tooth root and crown.
Researchers are also developing hybrid approaches that combine scaffolds with bioactive molecules to guide regeneration in situ (inside the mouth). While full human tooth regeneration remains a complex goal, stepwise advances in pulp regeneration and root formation are already influencing how endodontists and oral surgeons approach difficult clinical cases.
3D printing and bespoke materials: faster, more precise restorative care
Digital and additive manufacturing (3D printing) have rapidly transformed restorative dentistry. Modern chairside and lab-based printers can produce crowns, bridges, surgical guides and even denture bases with a level of fit and surface quality that was difficult to achieve a decade ago. Advances in materials science — including biocompatible resins and ceramics and improved sintering processes — have reduced production times and increased durability, allowing clinics to offer same-day restorations more often.
More experimental but striking innovations include low-temperature, biomaterial-based printing tools that can deposit bone-like scaffolds during surgery, improving bone repair and implant site preparation. These kinds of intraoperative printing devices aim to conform precisely to irregular defects and can be loaded with antibiotics or growth factors to accelerate healing — innovations that may make complex implant surgeries quicker and more predictable.
For practices, 3D printing means streamlined workflows: digital scans link directly to CAD software and printers, reducing remakes and improving patient communication through visual previews. For patients, the advantage is better-fitting, faster, and increasingly affordable dental prosthetics.
AI, imaging and tele dentistry: smarter diagnostics and wider access
Artificial intelligence is moving from research labs into everyday dental practice. Machine-learning tools now assist clinicians like Smile Hub Dublin by analysing radiographs, intraoral scans and photos to detect caries, periodontal bone loss and other pathologies with increasing sensitivity and speed. AI models trained on large datasets can flag early enamel lesions, identify periapical infections and help plan implant placements. In parallel, tele dentistry platforms have integrated AI triage systems that support remote screening, making it easier for underserved or mobility-limited patients to get timely advice.
AI also improves workflow efficiency: automated charting, image annotation and treatment-planning suggestions free clinicians to spend more time on patient care rather than admin. Importantly, these systems are decision-support tools and do not replace clinical judgement. Ongoing studies continue to validate performance across different populations and imaging devices.
Biomaterials and remineralisation: preventing and reversing decay
Preventive science has advanced as well. Rather than waiting for cavities to form and filling them, researchers are developing therapies that encourage enamel and dentine remineralisation. Self-assembling peptides, casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) formulations, and novel fluoride-releasing bioactive glasses have shown promise in re-mineralising early carious lesions and strengthening demineralised tooth structure.
Clinical results are nuanced: some peptide-based products have demonstrated significant remineralisation in certain studies, whereas others have produced mixed results depending on the tooth type and lesion severity. The takeaway for clinicians is that remineralisation protocols — combined with patient-level prevention (dietary advice, fluoride use and oral hygiene) — are increasingly viable first-line strategies for managing early decay without invasive restorations.
Microbiome and host-modulation therapies
Another frontier is manipulating the oral microbiome and host responses to control disease. Instead of broad-spectrum antimicrobials, targeted approaches aim to reduce pathogenic bacteria while preserving beneficial species. Researchers are testing probiotic formulations, bacteriophage therapies and small molecules that dampen destructive inflammation in periodontal disease. Host-modulation strategies — drugs or biologics that modify the immune response — could limit tissue destruction in aggressive periodontitis and improve outcomes when combined with mechanical therapy.
Although many of these interventions are experimental, they reflect an important shift: treating the microbial ecology and inflammatory drivers of disease, not just removing biofilm mechanically.
Minimally invasive and patient-centred care
Across these technical advances is a broader clinical trend towards minimally invasive, patient-centred care. Techniques such as atraumatic restorative treatment (ART), selective caries removal, adhesive restorations and guided tissue regeneration allow clinicians to preserve more natural tooth structure and reduce patient discomfort. Combined with digital planning and local anaesthesia improvements, procedures that once required multiple visits can now be completed more quickly and with less postoperative pain.
Furthermore, personalised risk assessment — informed by genetic markers, microbiome profiles and lifestyle data — helps tailor prevention and treatment strategies to the individual rather than applying blanket protocols.
Regulatory hurdles, cost and evidence base
It is important to be realistic. Many of the most exciting technologies are at different stages of development: some are widely available (digital scanning, CAD/CAM restorations, certain AI diagnostic tools), while others remain in clinical trials (stem-cell therapies, microbiome modulation, intraoperative biomaterial printers). Regulatory approval, long-term safety data, reproducibility across diverse patient groups and cost-effectiveness analyses are essential before widespread adoption.
Clinicians should therefore balance innovation with caution: adopt proven technologies that enhance care today, but watch the evidence for emerging options and ensure patients understand experimental aspects of new treatments.
What this means for patients and clinicians
For patients, the net result is better outcomes, faster care and more options. In the near future we can expect more same-day restorations, greater use of biologically based repairs for early disease and improved access through tele dentistry and AI triage. For clinicians, the landscape rewards lifelong learning: understanding digital workflows, interpreting AI outputs, and integrating new biomaterials will become core competencies.
Ultimately, dental care is becoming more predictive, preventive and restorative in a biological sense — not just prosthetic. As research continues and technologies mature, many routine problems may be managed with less invasive, more natural solutions.
Final thoughts
The latest breakthroughs in dental treatment reflect a convergence of biology, materials science and digital technologies. While not every promising idea will become mainstream, the direction is clear: dentistry is evolving from mechanical repair to intelligent, biologically driven care that prioritises preservation and regeneration. Patients should expect safer, faster and more personalised dental journeys in the years ahead — but clinicians must remain guided by robust evidence and best practice as these innovations are translated into everyday care.