Executive Summary
Liver disease is currently the second leading cause of years of working life lost in Europe, second only to ischaemic heart disease1. An analysis of the interaction between patients with cirrhosis with ascites (CwA), caregivers, and healthcare providers has shown a need to improve patient-physician coordination and guidance on lifestyle changes. Addressing the stigma associated with cirrhosis is essential in discussions about the disease and its treatment and may influence patient health behaviours2. We therefore sought to develop and validate a patient Toolkit that could be used by patients to highlight specific concerns to be discussed during consultations with their healthcare team, both at first visit and at follow-up appointments.
During the four-step development of the Toolkit, in collaboration with UK hepatologists and patient advisory group representatives, key topics for discussion during consultations were identified. The Toolkit questionnaire, encompassing a range of questions covering the physical and psychological aspects of CwA, was developed and refined based on these key topics. This questionnaire was validated through additional consultations with hepatologists and specialist nurses across Europe (Spain, Italy, Germany). The healthcare providers involved in the validation process found these questions to be important in addressing the comprehensive care of patients with CwA. Henceforth, we will refer to this comprehensive resource as the ‘Toolkit’.
Regarding the implementation of the Toolkit, discussions concluded that handing a paper version directly to the patient with CwA is the most efficient approach to ensure Toolkit completion before their visit. However, this approach may need to be adapted according to local guidelines and limitations, and individual patient requirements. Endorsement for the Toolkit has been provided by two patient associations involved in its development: the British Liver Trust and Liver4Life, with the aim of increasing patient and caregiver trust in the Toolkit.
Introduction
Cirrhosis has a prevalence of approximately 800 per 100,000 inhabitants and causes approximately one million deaths annually worldwide. 3 Europe has the largest burden of diagnosed liver disease in the world, and this burden continues to grow. 4 Patients with cirrhosis have significant physical, psychological, and practical needs that need to be considered during their management. 3,5 Previous research conducted by Grifols on the experience of patients with cirrhosis has highlighted that patients feel little can be done about their condition, resulting in a lack of active disease management and reduced engagement with their healthcare providers, potentially leading to a decline in their health and increased feeling of isolation. This research has identified both poor coordination of care and guidance provided to patients, and highlighted the detrimental effects of stigma and discrimination, as challenges in the management of cirrhosis with ascites (CwA). Healthcare providers reported frustration both at the disjointed nature of services provided, and with the difficulty patients encountered with compliance to treatment regimens. Conversely, patients reported a more positive response to direct instructions (e.g., specific guidance on how to adopt a low-salt diet). Regardless of their disease aetiology, patients often report feeling stigmatised due to preconceptions about cirrhosis,6 resulting in a lower likelihood of seeking medical care or receiving support.7 Analysis of the interaction among patients, caregivers, and healthcare providers highlighted the need to enhance a coordinated approach and provide information to patients about their condition. 3 The timing, frequency, and content of patient visits may pose further challenges for patients. Consultations with hepatologists typically last an average of 20 minutes, with follow-up appointments generally scheduled every three to six months. Exceptions are only made for emergent or complex 3 cases. Discussions usually include lifestyle, medication, and patient adherence to recommendations. Test results and the need for follow-up tests are also discussed, but more personal topics (e.g., sleep disorders, diet and personal relationships) tend to be, albeit rarely, discussed with nurses.
Given the challenges faced by patients and healthcare providers, we sought to: improve communication between patients with CwA and their hepatologists during hospital visits, enhance the patient and healthcare provider experience, facilitate coordination, and ultimately, improve disease management. In collaboration with both patient advisory group representatives and hepatologists across Europe, we developed and validated a Toolkit to improve the flow of information between patients and healthcare providers.
Toolkit development
In a four-step approach that involved close consultation with healthcare providers and patient advisory groups, key topics were identified and discussed, and the Toolkit questionnaire was developed.
Firstly, an internal workshop was conducted to incorporate current knowledge and expertise in the setting of CwA and to fully understand where the Toolkit could aid both current and future CwA care pathways. Online discussions were then conducted with UK patient advisory group representatives (n=3) and UK hepatologists with experience in treating patients with CwA (n=3). This gave the opportunity for unfiltered feedback on each of their needs and any frustrations regarding the management of patients with CwA. These discussions allowed the identification of key themes, common frustrations, and unmet needs.
Themes that emerged during the hepatologist (n=3) and patient advisory group representatives (n=3). CG, caregiver; GP, general practitioner; HCP, healthcare provider; PAG, patient advisory group; QoL, quality of life.
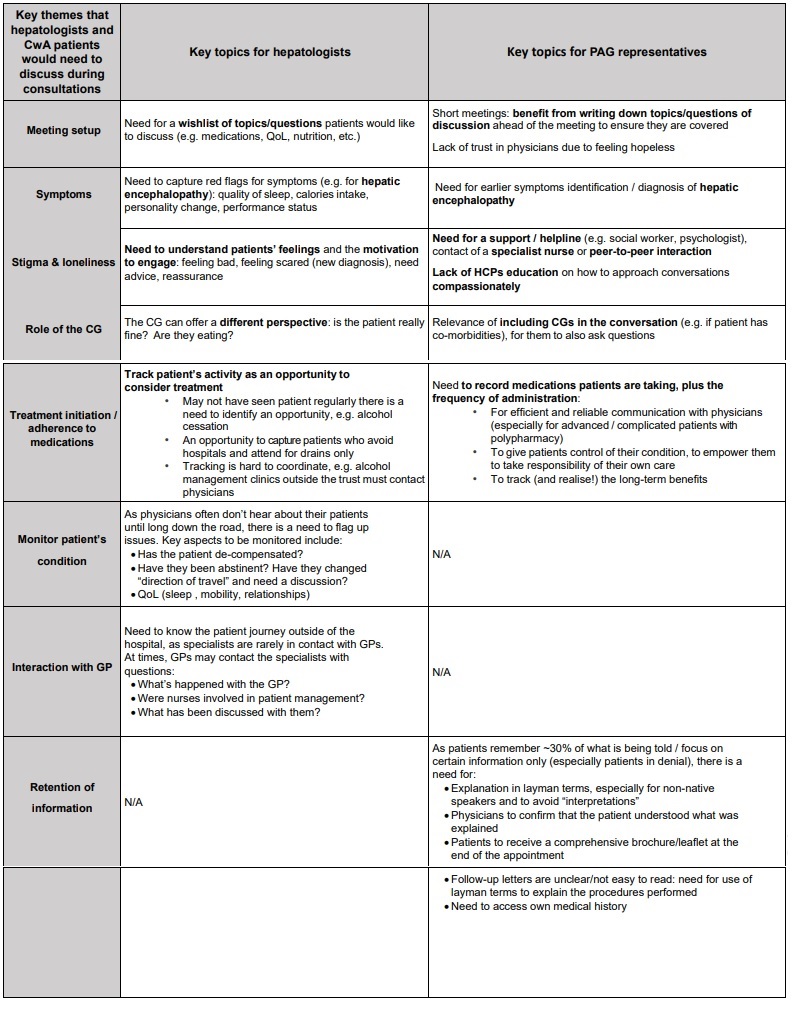
The common themes that emerged included ‘Meeting setup’, ‘Symptoms’, ‘Stigma and loneliness’, ‘Role of the caregiver’, ‘Treatment initiation/adherence to medications’, ‘Monitoring the patient’s condition’, ‘Interaction with the GP’, and ‘Retention of information’. In terms of priority, hepatologists positioned the need for a wishlist of topics/questions patients would like to discuss (i.e. ‘Meeting setup’) as the most important, whereas the patient advisory groups ranked ‘Stigma and loneliness’ as the most important. These themes were then discussed in three one-hour sessions that brought together all patient advisory group representatives and hepatologists to identify the questions that would be included in the Toolkit. Lastly, in a 90- minute workshop, the Toolkit was further reviewed and refined and ways that the Toolkit could be implemented in clinical practice were discussed. Following this final workshop, a first full draft of the Toolkit was developed, and a strategic plan for its implementation was defined.
The discussion Toolkit presenting a comprehensive overview of the consultation topics.
 Toolkit Validation
Toolkit Validation
Toolkit validation and implementation into clinical practice across Europe could be important steps in facilitating better communication between patients with CwA and their physicians. Following the development of the draft Toolkit, there was a need for validation to ensure its optimal use in specialist centres. It was also important to understand how to implement the Toolkit in clinical practice and to maximise its use across centres.
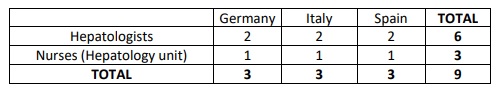
To validate the Toolkit, hepatologists and specialist nurses were recruited across Germany, Italy, and Spain.
Sample of hepatologists and nurses recruited across Europe for interviews to validate the CwA Toolkit.
Eligible hepatologists were involved in the diagnosis, treatment, and management of at least 30 adult patients with CwA, while nurses were recruited from the same centers and were required to be actively involved in the management of these patients. Selected hepatologists and nurses worked in the same clinical unit in key centres of interest. Once recruited, 30-minute in-depth interviews were conducted with each hepatologist and nurse.
Overall, reactions to the Toolkit were positive with feedback confirming that the questions covered key areas of importance. The feedback generally reported an accurate representation of topics on the physical and psychological aspects of CwA that were usually discussed during consultations. It was noted that hepatologists are more interested in clinically focussed questions. However, the topic of emotional wellbeing is considered important, as it impacts on patient attitude, lifestyle, compliance to treatment, diet and
disease management. Nurses tended to visit patients with CwA more frequently and for longer periods of time, especially if conducting paracentesis. In these situations, the Toolkit would be less relevant. However, the nurses agreed that the included topics were essential, as patients may feel overwhelmed at consultations with undiscussed concerns, which are often only addressed with nurses at a later stage. One nurse noted the potential benefits that the Toolkit could offer to caregivers, for instance, in capturing valuable information about the patient, while making them feel that their efforts are recognised.
Implementation
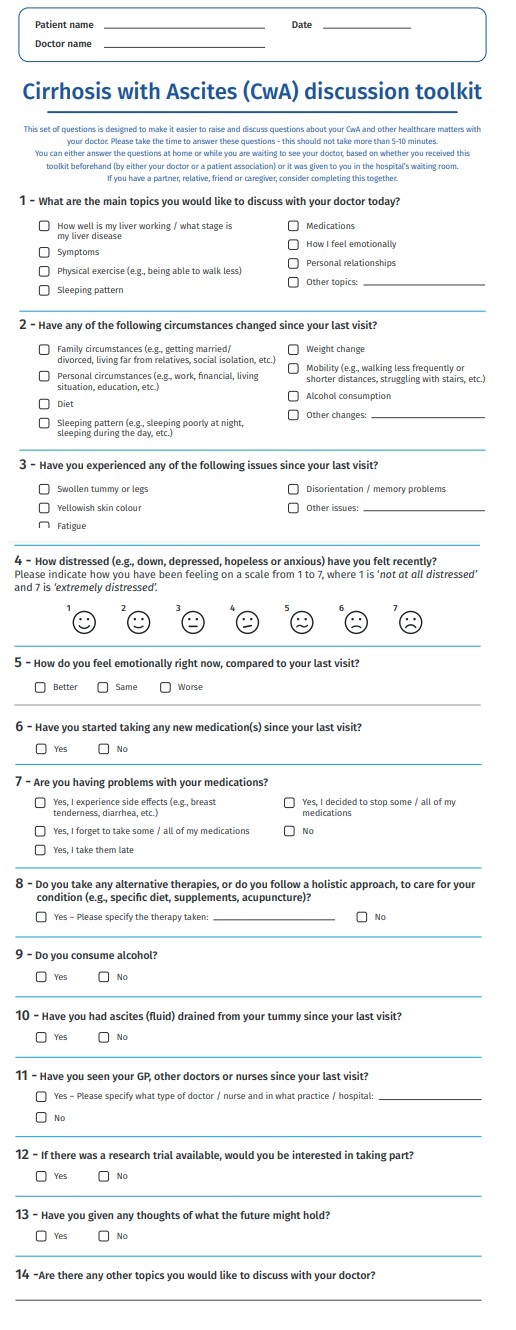
The validated Toolkit for patients with CwA was developed to improve the communication between CwA patients and their hepatology team. A useful Toolkit would be one that is readily available at every visit, that takes 5–10 minutes to complete prior to the visit, and that encourages communication of non-emergency issues.
The Toolkit provides an opportunity for patients and carers to report where they need additional support and to coordinate advice received from services outside the hospital setting. It can also help raise concerns that may need further exploration, such as advice on managing treatment side effects, diet, and participating in a trial. It is also hoped that patients will feel an increased sense that their concerns are visible to their care team.
In terms of practical implementation of the Toolkit, discussions concluded that providing a paper version to patients with CwA in the waiting room before their consultation would be the most efficient way to ensure completion ahead of speaking with their hepatologist. However, the Toolkit could also be handed to the patient by the hepatologist at their visit or sent electronically via email or text message. The patient would then complete the Toolkit, before their consultation, to be reviewed and discussed with their healthcare team. The
completed Toolkit would then be scanned and added to the patient’s health records.
This implementation approach may need to be adapted according to local guidelines and limitations. For example, while the patient is welcomed by a receptionist in most centres, electronic registration is performed in others. In these cases, the Toolkit would need to be handed to the patient by a nurse or physician during the consultation. Also, as the completed Toolkit would need 8 to be scanned (if completed on paper) and added to the patient’s electronic records, some centres might find it challenging to identify a dedicated team member for this task. Another consideration is the potential requirement of
local ethical committee approval and patient consent at the collection of personal information. Completion of the Toolkit could be challenging for some patients, which might necessitate a longer time to complete it, potentially with the aid of a nurse or carer.
Next Steps
Several steps are recommended to enhance and expedite the implementation and dissemination of the Toolkit. Firstly, establishing a clear communication plan to inform healthcare providers, patients and carers about the Toolkit’s availability and benefits. This would involve the creation of information materials, including leaflets or digital content. Secondly, to ensure effective use, the development of training sessions for healthcare professionals would be required. This training would focus on the Toolkit’s features, its role in improving patient-provider communication, and the potential positive impact on patient outcomes. A potential future step could involve piloting the Toolkit in specialist centres or ‘Centres of Excellence’ to explore the improvements it may offer to consultations between patients and hepatologists.
Research with patients, caregivers, and healthcare providers would be ongoing to collect feedback on the use and implementation of the Toolkit in real-world settings, facilitating refinements and improvements if necessary. It’s important to note that the Toolkit will be launched independently of the pilot.
Acknowledgments
Medical writing assistance was provided by RubyDuke Communications, with financial support from Elma Research.
References
1. Karlsen TH, et al. Lancet. 2022 Jan 1;399(10319):61–116.
2. Schomerus G, et al. J Hepatol. 2022 Aug;77(2):516–524.
3. Hjorth M, et al. PLoS ONE 2023;18(4):e0283611.
4. Pimpin L, et al. J Hepatol 2018;69(3):718–735.
5. Valery PC, et al. Hepatol Commun 2021;5(5):891–905.
6. Hjorth M, et al. J Clin Nurs. 2020;29(23–24):4532–4543.
7. Vaughn-Sandler V, et al. Dig Dis Sci 2014;59(3):681–686.