The Zika virus is considered a major global health risk, as infection during pregnancy is associated with babies born with microcephaly.
The 2014 Ebola outbreak in West Africa killed over 11,300 people, despite not being spread through the airborne route. The 2016 Yellow Fever outbreak in Angola killed 159 people and the outbreak in Brazil killed 261 people, despite having a vaccine available that is highly effective.
What about a virus that can spread through the airborne route, survive on hard surfaces for 24 – 48 hours, can increase a child’s risk of bipolar disorder if the mother is infected while pregnant, can increase risk of fetal death and still birth during pregnancy, and can worsen chronic medical conditions such as asthma, diabetes and heart disease?
A novel pathogen with these features will definitely be on the news. In fact, a virus with these characteristics exists and gets featured in the news once a year –during the colder half of the year in each hemisphere, late November through to March in the Northern Hemisphere and April to October in the Southern Hemisphere. This virus is the good old influenza (or the flu). Most people group the flu and colds together and refer to the “cold and flu season”. Some consider flu infection as “normal” or customary while some are convinced that they “never get the flu”.This is far from the truth –influenza is nothing like the cold!
Influenza is the most lethal viral pandemic in history
Influenza is one of humanity’s most persistent and constant foes and no virus can claim credit for more worldwide pandemics than influenza. The outbreak of the Spanish flu in 1918 is generally considered to be one of the worst pandemics in human history, infecting 20 to 40 percent of the world’s population and killing 50 to 100 million in a span of just two years. The 1957 “Asian flu” was first identified in China, whereby it caused around 2 million deaths.
This severe strain emerged when a human form of H2N2 combined with a mutant strain in ducks. The 1968–69 “Hong Kong flu” was first detected in Hong Kong where it killed 1 million people. The most recent flu pandemic had its origins in Mexico. The “Swine flu” was a combination of a Eurasian swine flu with another strain that was a mix of both bird and human flu virus. This strain killed 18,000 people globally and as many as 89 million people were infected worldwide.

Anyone can get infected with the flu
Anyone can get infected with the flu, including healthy people, and complications related to the flu can happen at any age, especially in pregnant women, the very young (less than 2 years old), older adults, and people with chronic medical conditions (diabetes, heart problems, asthma, chronic obstructive pulmonary diseases, cancer, HIV) and other conditions that impair or weaken the immune system.
Influenza cases and deaths: “Tip of the Iceberg”
A 2014 study published in Lancet Respiratory Medicine showed that only 17% of the symptomatic cases confirmed by nasal swab analysis saw a doctor for flu. A 2016 study in New Zealand reported that 80% of people who were infected with the flu in the past season did not see a doctor and most did not even know they were infected. These studies show high rates of influenza infection in the community and the reported cases are just the tip of the iceberg, with a large invisible clinical and sub clinical iceberg not recorded by routine influenza surveillance.

Influenza is an effective trigger for other diseases. It can cause a wide range of complications, including pneumonia (lung infection), bacterial co-infection, ear infections, inflammation of the heart (myocarditis), brain (encephalitis) or muscle (myositis, rhabdomyolysis) tissues, multi-organ failure, worsening of asthma, diabetes and heart disease.Because people with asthma have sensitive airways, the flu can cause further inflammation of the airways and lungs, provoke an asthma attack or worsen symptoms. In patients with diabetes, the flu interferes with glucose management, putting people, especially those with type 1 diabetes, at an increased risk of diabetic coma. The flu can trigger a heart attack in patients with heart disease and up to half of unexpected influenza deaths are due to heart disease.
Cancer patients and people with HIV/AIDS, who have compromised immune systems, are at a greater risk of developing serious flu-related complications, which can result in death. The World Health Organization (WHO) estimates that influenza epidemics result in about 250,000 to 500,000 deaths yearly. This is a conservative estimate because deaths due to pneumonia, stroke or diabetes that were actually triggered by the flu are not recorded as flu deaths.
Flu-conomics: the economics of influenza
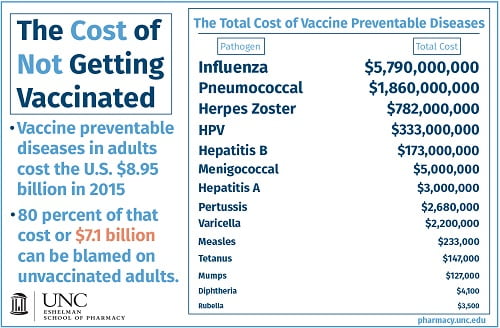
Influenza costs are classified as direct costs (treatment fees, hospital charges), or indirect costs (work absenteeism, decreased performance, premature death). Influenza infection is stressful for the sick and for those taking care of the sick individual. The socio-economic impact of influenza is difficult to quantify but, for older individuals, flu infection is associated with a decline in major physical functions. According to the US Centers for Disease Control and Prevention, the flu costs more than $87 billion annually. Flu outbreaks can mean lost sales opportunities, reduced workforces, backlogged tasks, customer service issues, or all the above.
In the US, 65% of the estimated annual economic burden, equivalent to $5.8 billion, in health-care costs and lost productivity resulted directly from influenza. In the UK, sick leave costs employers a total of £29 billion annually. In Australia this year, the flu epidemic was estimated to have cost $47.8 million in lost productivity in the month of August alone.
There is some good news: good health habits like washing hands and covering the mouth and nose when coughing or sneezing can help stop the spread of the flu. But getting an annual flu shot is the single best way to protect people from the flu.
Melvin Sanicas, MD MSc FRSPH
Dr Melvin Sanicas is a vaccinologist and public health physician with over 10 years international experience in drug and vaccine development, regulatory affairs, and drug safety. He was a Global Health Fellow and Program Officer at the Bill & Melinda Gates Foundation where he launched the Collaboration for TB Vaccine Discovery and managed a portfolio of over US$ 20M of research and capability building projects in Europe, US, and Africa. Dr Sanicas is a partner at the Brighton Collaboration, a Fellow of the Royal Society of Tropical Medicine and Hygiene, and a Fellow of the Royal Society for Public Health.


















