Revolutionizing Oral Drug Delivery with Nanotechnology
The pharmaceutical landscape stands at a transformative juncture where nanotechnology oral drug delivery systems are reshaping how medications reach their therapeutic targets. This convergence of nanoscience and pharmaceutical formulation addresses fundamental challenges that have long plagued drug development, offering solutions to poor bioavailability, limited solubility, and inadequate therapeutic efficacy that characterize many promising drug candidates.
The Bioavailability Challenge in Modern Pharmaceutics
Oral administration remains the most preferred route for drug delivery, valued for its safety, convenience, lower costs, and high patient compliance. Yet this route presents formidable obstacles. The biological permeability and water solubility of drugs pose substantial barriers to effective oral drug delivery. Solubility determines the amount of drug that can be dissolved in solution, while permeability governs the ability to traverse biological membranes, ultimately determining therapeutic efficacy and safety.
Over 70% of new drug candidates demonstrate low solubility values in water, with approximately 40% of lipophilic drug candidates failing to reach market because low aqueous solubility compromises bioavailability and leads to poor pharmacokinetic performance. The gastrointestinal environment further complicates matters through pH variations, enzymatic activity, and the mucus barrier, all of which may affect the dissolution or absorption of therapeutic drugs.
When drugs are administered orally, they encounter a complex series of biological barriers. The process begins with dissolution in gastrointestinal fluids, followed by permeation across the mucus layer, transit through the intestinal epithelium, and evasion of first-pass hepatic metabolism. Each stage presents opportunities for drug loss or degradation, reducing the fraction of administered dose that ultimately reaches systemic circulation.
Nanoparticle Innovation Transforming Drug Delivery
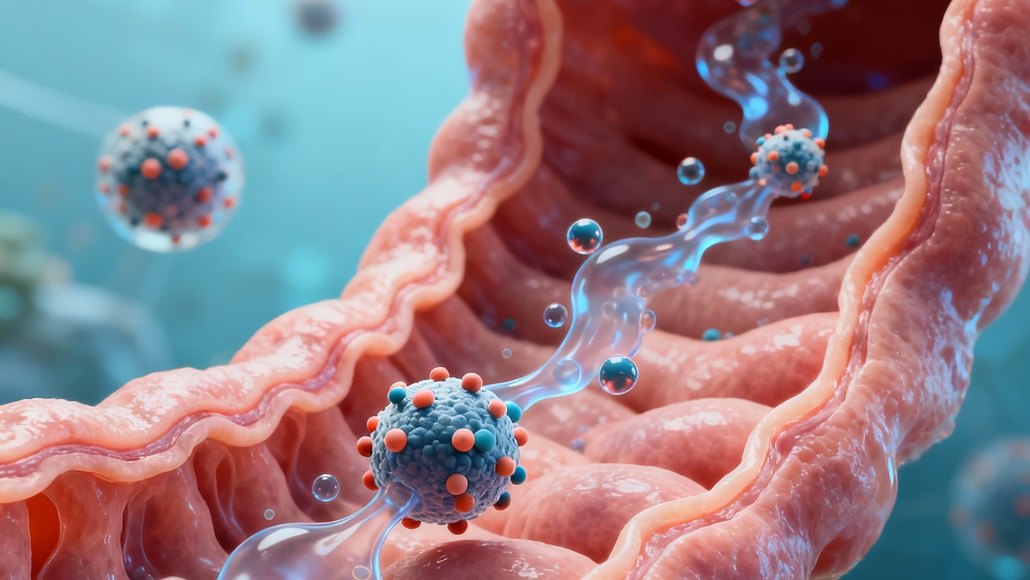
Nanotechnology oral drug delivery systems leverage the unique physiochemical properties of nano-sized materials and structures to overcome traditional limitations. Nanoparticles, typically ranging from 1 to 300 nanometers in size, fundamentally alter drug solubility, cellular absorption, membrane permeability, and biodistribution within the body. This nanoscale dimension is not merely a reduction in size but represents a paradigm shift in how drugs interact with biological systems.
The advantage of using nanotechnology lies in the remarkable properties that emerge at the nanoscale. Numerous aspects, including drug solubility, cellular absorption, membrane permeability, and biodistribution within the body, can be impacted by the size of nanoparticles. When drug particles are reduced to nano size, they provide greater surface area and stronger contact with the solvent, which increases drug dissolution. This expanded surface area facilitates more substantial interactions with biological fluids, translating to enhanced solubility and absorption.
Nanoparticulate drug delivery systems have become a focal point of pharmaceutical research because of their unique advantages in protecting drugs from premature degradation, enhancing absorption through extensive surface area, and facilitating targeted administration of medications to specific regions. Through encapsulation, nanocarriers increase drug stability and protect therapeutic agents from the hostile gastrointestinal environment. The expanded surface area allows for improved interaction with absorptive surfaces, while the nanoscale dimensions enable cellular uptake through mechanisms unavailable to larger particles.
Mechanisms of Enhanced Bioavailability Through Nanotechnology
The enhancement of oral bioavailability through nanotechnology oral drug delivery operates through multiple complementary mechanisms. Size-dependent effects play a crucial role, as control of particle dimensions under 200 nanometers results in preferential absorption by the gastrointestinal tract. Smaller nanoparticles demonstrate improved bioadhesion in the gastrointestinal tract, which prolongs residence time and contributes to enhanced oral bioavailability. Research has demonstrated that when particle size decreases from approximately 329 nanometers to 89 nanometers, oral bioavailability can increase threefold, proving that particle size exerts a critical influence on oral drug delivery.
Surface properties of nanoparticles profoundly impact their interaction with biological pathways and alter efficacy. The surface chemistry can determine whether nanoparticles adhere to superficial layers of mucus and undergo rapid clearance, or whether they penetrate through the mucus barrier to reach absorptive epithelium. Modification with polymers such as polyethylene glycol creates a hydrophilic coating that reduces mucus adhesion and enhances penetration. Studies have shown that nanoparticles as large as 500 nanometers, when sufficiently coated with muco-inert polymers, can rapidly traverse physiological human mucus with diffusion rates only four times slower than in pure water.
The shape and geometry of nanoparticles also significantly impact oral bioavailability. Rod-shaped nanoparticles have demonstrated better oral bioavailability compared with spherical particles, as the geometry influences cellular uptake mechanisms and mucus penetration. Nanoparticle geometry affects circulation time, biodistribution, and cellular internalization, with elongated particles often showing advantages in navigating the complex architecture of biological barriers.
Advanced Nanocarrier Systems for Oral Delivery
Multiple types of nanocarriers have emerged as promising platforms for nanotechnology oral drug delivery. Polymeric nanoparticles, constructed from biodegradable polymers, offer versatility in encapsulating both hydrophilic and hydrophobic drugs. Chitosan, a naturally derived polysaccharide, represents a particularly valuable material for oral delivery due to its biocompatibility, mucoadhesive properties, and ability to transiently open tight junctions between epithelial cells. At low pH, chitosan protonation occurs, destabilizing tight junctions and increasing paracellular absorption. Chemical modifications like methylation can extend these properties and increase chitosan solubility across a broader pH range.
Solid lipid nanoparticles combine the advantages of polymeric nanoparticles with the benefits of lipid-based formulations. These systems demonstrate ability to improve oral bioavailability through enhanced solubility, protection from degradation, and facilitation of lymphatic transport for highly lipophilic drugs. The lipid composition can be tailored to optimize drug loading, release kinetics, and absorption pathways, providing formulation scientists with considerable flexibility.
Cyclodextrin-based nanoparticles exploit the unique cavity structure of cyclodextrin molecules to form inclusion complexes with poorly soluble drugs. The cyclodextrin cavity is large enough to accommodate guest molecules yet small enough to reduce contact between water and nonpolar regions of both host and guest. This inclusion complex formation represents an effective mechanism for increasing solubility. Cyclodextrin complexation has been utilized extensively to increase solubility and enhance bioavailability, with the added benefit of blocking efflux pump activity that would otherwise limit drug absorption.
Vesicular systems, including liposomes and niosomes, offer another avenue for nanotechnology oral drug delivery. These lamellar structures with aqueous compartments surrounded by amphiphilic molecules can deliver both hydrophilic drugs (encapsulated in the aqueous core) and hydrophobic drugs (incorporated into the lipid bilayer). Non-ionic surfactants used in niosomes provide capacity to improve solubility and enhance bioavailability of water-insoluble drugs.
Overcoming Biological Barriers
The gastrointestinal tract presents multiple obstacles that nanotechnology oral drug delivery must overcome. The mucus barrier, a viscoelastic gel layer covering epithelial surfaces, serves as the first line of defense. Mucus rapidly turns over, with clearance times ranging from minutes to hours depending on anatomical location. Conventional nanoparticles typically become trapped through steric or adhesive forces and undergo rapid elimination via mucus clearance mechanisms.
Nanoparticles address this challenge through two primary strategies. Mucoadhesive nanoparticles are designed to resist transit through the gastrointestinal tract by adhering to the mucus layer, extending residence time to match the timescale of mucus renewal. Chitosan exemplifies this approach, with its positive charge enabling electrostatic interactions with negatively charged mucins. The alternative strategy employs mucopenetrating nanoparticles, engineered to avoid adhesion and rapidly traverse the mucus layer before clearance. Surface modification with polyethylene glycol or similar hydrophilic polymers creates a protective corona that prevents mucin interaction.
Beyond the mucus barrier, nanoparticles must navigate the intestinal epithelium, a tightly regulated barrier controlling molecular passage from the lumen to systemic circulation. Nanoparticles exploit multiple transcellular and paracellular routes. Transcellular pathways include passive diffusion, receptor-mediated endocytosis, and specialized uptake through M cells overlying Peyer’s patches. The nanoscale dimensions of these carriers enable cellular uptake mechanisms unavailable to larger particles or free drugs.
Efflux transporters, particularly P-glycoprotein, pose another significant barrier by actively pumping absorbed drugs back into the intestinal lumen. Certain nanoparticle formulations can inhibit efflux pump activity, either through direct interactions with transporter proteins or by overwhelming the capacity of these systems. Some excipients used in nanoparticle formulations, including surfactants and polymers, demonstrate intrinsic P-glycoprotein inhibitory effects that complement the benefits of nanoencapsulation.
Protection and Stability Enhancement
A critical advantage of nanotechnology oral drug delivery lies in protection of therapeutic agents from degradation. The gastrointestinal tract represents a harsh environment with extreme pH variations, enzymatic activity, and oxidative stress. Many promising drug candidates, particularly biologics and peptides, undergo rapid degradation when exposed to gastric acid or intestinal enzymes.
Nanoencapsulation provides physical barriers that shield drugs from these environmental challenges. By encapsulating medications in nanoparticles, formulations can be made more soluble and bioavailable while better able to target particular gastrointestinal sites and maintain stability in the harsh gastrointestinal environment. The drug remains protected along the gastrointestinal tract within the nanoparticle matrix, preserving high concentrations of active drug at absorption sites and enabling faster absorption compared to conventional formulations.
The protective effect extends beyond chemical stability to include physical stability. Nanoencapsulation prevents aggregation of poorly soluble drugs, maintaining them in a finely dispersed state that maximizes surface area for dissolution. This is particularly valuable for drugs that tend to crystallize or aggregate in aqueous environments, as the nanoparticle matrix prevents molecular self-association.
Formulation Strategies and Optimization
Successful development of nanotechnology oral drug delivery systems requires careful consideration of multiple formulation parameters. Drug loading capacity must be optimized to deliver therapeutic doses in reasonable volumes while maintaining nanoparticle stability. Higher drug loading can be achieved through selection of appropriate polymers or lipids with favorable drug-carrier interactions, though excessive loading may compromise particle stability or release characteristics.
Release kinetics represent another critical design parameter. Controlled release formulations can maintain proper therapeutic concentrations over extended periods, reducing dosing frequency and improving patient compliance. Release can be triggered by environmental factors such as pH changes along the gastrointestinal tract, allowing targeted delivery to specific intestinal segments. Alternatively, release may be governed by polymer degradation rates or diffusion through the nanoparticle matrix, providing sustained drug exposure.
Scalability and manufacturability considerations influence formulation design from early development stages. Methods such as nanoprecipitation, emulsion techniques, and spray drying must be adaptable to industrial-scale production while maintaining consistent nanoparticle characteristics. Recent advances in continuous manufacturing processes offer improved control over particle size distribution and batch-to-batch reproducibility compared to traditional batch methods.
Clinical Translation and Regulatory Considerations
The translation of nanotechnology oral drug delivery from laboratory research to clinical products requires navigation of complex regulatory pathways. Regulatory agencies evaluate nanoformulations with particular attention to characterization of particle properties, stability, safety, and performance. Comprehensive characterization must demonstrate consistent particle size distribution, surface properties, drug loading, and release profiles across manufacturing batches.
Safety evaluation encompasses assessment of nanoparticle interactions with biological systems beyond traditional drug toxicology. Potential accumulation in tissues, immunological responses, and long-term effects of chronic exposure require investigation. While many nanoparticle systems utilize materials with established safety profiles such as approved polymers and lipids, the nanoscale dimensions may confer novel biological behaviors warranting additional scrutiny.
Despite regulatory complexities, numerous nanoformulations have achieved market approval and commercial success. These products validate the clinical potential of nanotechnology oral drug delivery and provide precedents guiding development of next-generation systems. The growing body of approved nanoformulations demonstrates feasibility of translating nanomedicine concepts into therapeutics that address unmet clinical needs.
Emerging Frontiers and Future Directions
The field of nanotechnology oral drug delivery continues to evolve with exciting innovations on the horizon. Smart or stimuli-responsive nanoparticles represent one frontier, with systems designed to release drugs in response to specific biological signals. These may include pH-sensitive formulations that take advantage of pH gradients in the gastrointestinal tract, enzyme-responsive systems that release drugs upon contact with specific digestive enzymes, or glucose-sensitive formulations for diabetes management.
Personalized nanomedicine approaches seek to tailor nanoparticle formulations to individual patient characteristics. Variations in gastrointestinal physiology, genetic factors affecting drug metabolism, and disease states can all influence nanoparticle performance. Advanced manufacturing techniques such as three-dimensional printing may enable on-demand production of customized nanoformulations optimized for individual patients.
Integration of targeting ligands represents another promising direction. By decorating nanoparticle surfaces with molecules that bind specific receptors on target cells, formulations can achieve enhanced cellular uptake and accumulation at disease sites. This approach is particularly valuable for drugs treating gastrointestinal diseases or for enabling oral delivery of biologics that require transcytosis across the intestinal barrier.
The convergence of nanotechnology with other advanced pharmaceutical technologies promises to unlock new therapeutic possibilities. Combination of nanoformulations with permeation enhancers, efflux pump inhibitors, or mucus-modifying agents may synergistically improve oral bioavailability. Integration of nanocarriers with microdevices or ingestible electronics could enable controlled release triggered by electronic signals or real-time monitoring of drug absorption.
Conclusion
Nanotechnology oral drug delivery stands as a transformative innovation addressing fundamental challenges in pharmaceutical science. By manipulating materials at the nanoscale, these systems enhance drug solubility, protect therapeutic agents from degradation, facilitate transport across biological barriers, and enable targeted delivery to specific gastrointestinal regions. The impressive body of research demonstrating improved bioavailability, enhanced therapeutic efficacy, and successful clinical translation validates the promise of this technology.
As the field matures, continued innovation in nanoparticle design, manufacturing processes, and regulatory frameworks will expand the impact of nanotechnology oral drug delivery. The technology offers particular value for addressing the growing pipeline of poorly soluble drug candidates and enabling oral administration of biologics traditionally limited to parenteral routes. With ongoing research and development, nanotechnology will continue revolutionizing oral drug delivery and improving patient outcomes across diverse therapeutic areas.